Foot Specialist / Chiropodist Services Thornhill, ON
Our Foot Specialist / Chiropodists at Foot Relief Clinic are equipped to handle all your Chiropody / Podiatry needs. Some of our leading services on this page.
| · Achilles Tendon
· Ankle Instability · Ankle Sprains · Arthritic Foot & Ankle Care · Athletes Foot · Bunions · Calluses · Corns · Crush Injuries · Diabetic Foot · Infections · Flat Feet |
· Fungus Toenails
· Geriatric Foot Care · Hammertoes · Heel Spurs · Ingrown Toenails · Injuries · Metatarsalgia · Neuromas · Orthotics · Plantar Fasciitis · Warts · Wounds |
Ankle Sprains Ankle sprains are caused by an unnatural twisting or force on the ankle bones of the foot, often resulting in one or more ligaments on the outside of the ankle to be stretched or torn. If not properly treated, ankle sprains could develop into long-term problems.
Bunions
Bunions are misaligned big toe joints that can become swollen and tender, causing the first joint of the big toe to slant outward, and the second joint to angle toward the other toes.
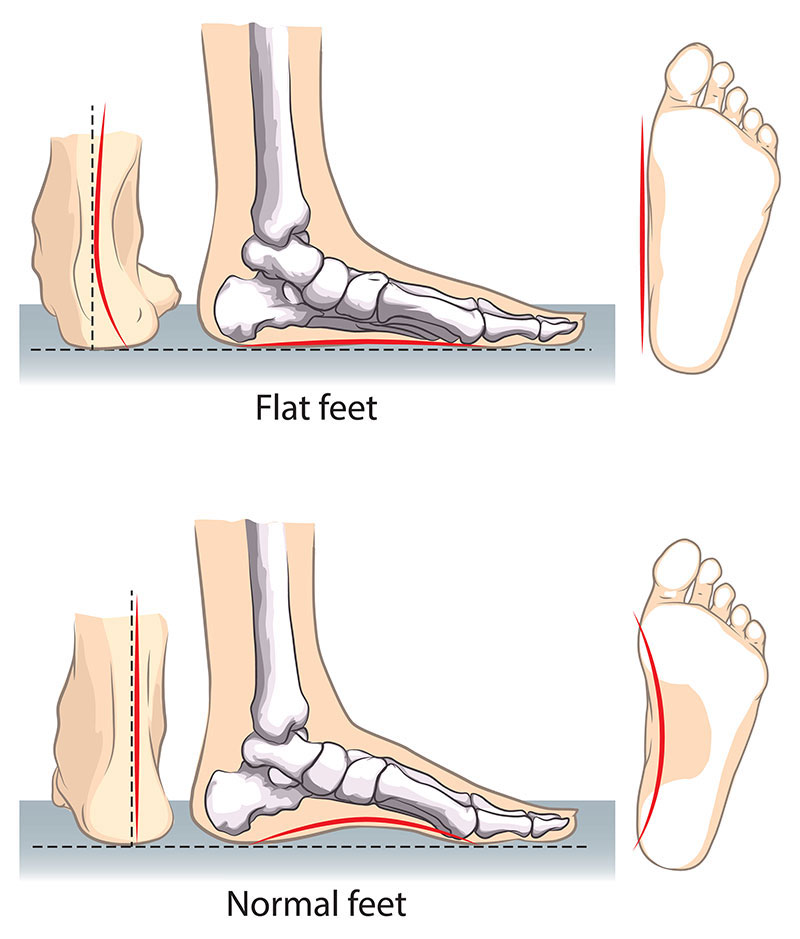
Flat feet are a common condition. In infants and toddlers, the longitudinal arch is not developed and flat feet are normal. The arch develops in childhood, and by adulthood, most people have developed normal arches.
Do you have Flat Feet? This happens with Adults and Children
Flat feet is defined as a postural superiority where the arches of the foot tend to collapse and the entire sole comes into complete contact with the ground. Some individuals have an arch of the foot in which it never develops in just one foot or both. A functional relationship exists between the biomechanics of lower leg and structure of arch of the foot. The arch provides a springy and elastic connection between the hindfoot and forefoot. The association moves forward by safeguarding as the majority of forces incurred during the weight bearing of the legs which will be dissipated before the long bones of thighs and legs experience the force associated with it.
The head of the talus bone, known as pes planus is distal from navicular and displaced medially. The tibialis posterior muscle tendons and the spring ligament gets stretched and so the individual with pes planus would lose the function of the MLA (medial longitudinal arch). The individual will have a rigid flatfoot if the MLA is nonfunctional or absent in both standings and in seated positions. If in case the MLA is functional and present while the individual is standing or sitting up on the toes, the person will tend to have a flexible flatfoot. Well-fitting arch supports will be used to correct this latter condition. The flat foot can be caused in children as well as for adults.
Children:
In infants, the appearance of the flat feet is quite common and normal which is due to the baby fat that masks the developing arch. In early childhood and infancy, the growth of human arch is very common and is a part of normal, tendon, muscle, bone growth and ligament. Walking barefoot on different terrain and foot training, especially the foot gymnastics will facilitate the formation and increase the growth of arches during childhood. The developed arch occurs by the end of 6 years to the maximum. Hypermobility and dyspraxia are some of the genetic musculoskeletal conditions which are considered as symptoms for flat feet.
Ligament laxity is one of the factors associated with flat foot and so the shoe-wearing children associated with ligament laxity have a greater chance of developing arches compared to other shoe wearing children. The children who walk barefoot will also have an increased chance of developing more human arches. So instead of using flip flops and sandals, it is better to use closed-toe shoes.
Adults:
Development of flat foot is common in adults due to illness, injury, prolonged or unusual stress to the foot, a fault in biomechanics, and also increases the chances with age. Women of over 40 years will experience flat foot and is common among them. The risk factors which increase the chances of developing arches after a certain age are diabetes, hypertension, and obesity.
Most flat feet do not cause pain and are asymptomatic. Flat feet was a physical health reason for rejecting services in the military. Treatment must be done if there is a pain anywhere in the lower leg, lower back and the knees. Treatment is done using orthoses which include foot gymnastics, arch support or other exercises which are recommended by a physical therapist.
Hammertoes
Hammertoe is a deformity of the second, third or fourth toes. In this condition, the toe is bent at the middle joint, resembling a hammer. Left untreated, hammertoes can become inflexible and require surgery.
Diabetes and Your Feet
With a diabetic foot, a wound as small as a blister from wearing a shoe that’s too tight can cause a lot of damage. Diabetes decreases blood flow, so injuries are slow to heal.
Heel Spurs
Plantar fasciitis (or heel pain) is commonly traced to an inflammation on the bottom of the foot. Our practice can evaluate arch pain, and may prescribe customized shoe inserts called orthoses to help alleviate the pain.
CORNS
Corns and calluses are protective layers of compacted, dead skin cells. They are caused by repeated friction from skin rubbing against bony areas or against an irregularity in a shoe. Corns ordinarily form on the toes and calluses on the soles of the feet.Read More…
ATHLETE’S FOOT
A chronic infection caused by various types of fungus, Athlete’s foot is often spread in places where people go barefoot such as public showers or swimming pools.Read More…
Heel Pain/Plantar Fasciitis in the Toronto, ON area
Plantar Fasciitis
Plantar fasciitis is the term commonly used to refer to heel pain and arch pain traced to an inflammation on the bottom of the foot. More specifically, plantar fasciitis is an inflammation of the connective tissue, called plantar fascia, that stretches from the base of the toes, across the arch of the foot, to the point at which it inserts into the heel bone. Overpronation is the most common cause of plantar fasciitis. As the foot rolls inward excessively when walking, it flattens the foot, lengthens the arch, and puts added tension on the plantar fascia. Over time, this causes inflammation.
Heel Spur “Heel Pain”
Also known as heel spur syndrome, the condition is often successfully treated with conservative measures, such as the use of anti-inflammatory medications, ice packs, stretching exercises, orthotic devices, and physical therapy. Note: Please consult your physician before taking any medications. In persistent cases, Diowave laser treatment may be used to treat the heel pain.
Ingrown nails are nails whose corners or sides dig painfully into the skin, often causing infection. They are frequently caused by improper nail trimming, but also by shoe pressure, injury, fungus infection, heredity, and poor foot structure.
Toenails should be trimmed straight across, slightly longer than the end of the toe, with toenail clippers. If they become painful or infected, contact our office. We may remove the ingrown portion of the nail, and if the condition reoccurs frequently, we may permanently remove the nail.
A callus, also known as hyperkeratosis, is an area of hard, thickened skin that can occur across the ball of the foot, on the heel, or on the outer side of the big toe. Although many consider them a skin problem, they are indicative of a problem with the bone.
Calluses form from repeated friction and pressure, as the shoe (or ground) rubs against a bony prominence (bone spur) on the toe or foot. The skin thickens in response to this pressure. Small amounts of friction or pressure over long periods of time cause a corn or callus. A great deal of friction or pressure over shorter periods of time can cause blisters or open sores. Calluses typically develop under a metatarsal head (the long bone that forms the ball of the foot). Calluses have painful nerves and bursal sacs (fluid-filled balloons that act as shock absorbers) beneath them, causing symptoms ranging from sharp, shooting pain to dull, aching soreness.
Calluses can be treated with over-the-counter callus removers, which use strong acids to peel this excess skin away after repeated application. Be careful using these products as they can cause chemical burns when misapplied or used in excess. Alternatively, treat calluses as follows: Begin by soaking the foot or feet in warm soapy water and gently rubbing away any dead skin that loosens. Next, use a pumice stone or emery board to file away the thickened skin. Apply a good moisturizer to the hardened areas to keep them softer and relieve pain. Nonmedicated corn pads or moleskin (a thin fuzzy sheet of fabric with an adhesive back) are available in stores and can relieve pain caused by calluses. However, use caution removing pads or moleskins to avoid tearing the skin.
If you need assistance relieving calluses, please contact our office. We can trim and apply comfortable padding to the painful areas. In more severe cases, we may prescribe medication to relieve inflammation, or inject cortisone into the underlying bursal sac to rapidly reduce pain and swelling.
A plantar callus forms on the bottom of the heel over time where one metatarsal bone is longer or lower than the others. This structure causes the one metatarsal to hit the ground first and with more force than it is equipped to handle. As a result, the skin under this bone thickens. In most cases, plantar calluses can be treated without surgery. In some recurring cases, however, a surgical procedure, called an osteotomy, is performed to relieve the pressure on the bone.
A condition called Intractable Plantar Keratosis (IPK) is a deep callus directly under the ball of the foot. IPK is caused by a “dropped metatarsal,” which happens when the metatarsal head drops to a lower level than the surrounding metatarsals and protrudes from the bottom of the foot. This results in more pressure being applied in this area and causes a thick callus to form. A dropped metatarsal can either be a congenital abnormality, a result of a metatarsal fracture, or a structural change that may have occurred over time.
You can prevent calluses by:
- Switching to better-fitting shoes or using an orthotic device to correct an underlying cause.
- Buying socks with double-thick toes and heels or nylon hose with woven cotton soles on the bottom of the foot.
Fungal Toenails in the Toronto, ON Area
Fungal nails refer to any number of fungal nail infections that can occur on the foot. Since fungal toenails are usually more resistant and more difficult to treat than Athlete’s Foot, topical or oral antifungal medications may be prescribed. Note: Please consult a physician before taking any medications. Permanent nail removal is another possible form of treatment for tenacious fungal nails.
What are the Causes of Nail Fungus Infection?
Nail fungus infections typically originate from fungi, such as yeasts and molds. In most cases, the fungal infections are caused by a specific group of fungi called dermatophytes. These fungi can live in the layer of dead skin around your nails.
The infection can be a result of family history of susceptibility, increasing age, poor health conditions, nail trauma, climate (warm, moist), exposure to infected nails (sports/ fitness and communal bathing areas), and tight shoes.
Infected nails become discolored, thickened and brittle, and in some cases, can interfere with daily activities.
Many of our clients who are suffering from Knee, Ankle or back pain find relief by using weight loss diet as well
For more information regarding Weight loss Diets
PLEASE CLICK